
Medical image Segmentation
What is medical image segmentation?
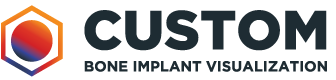
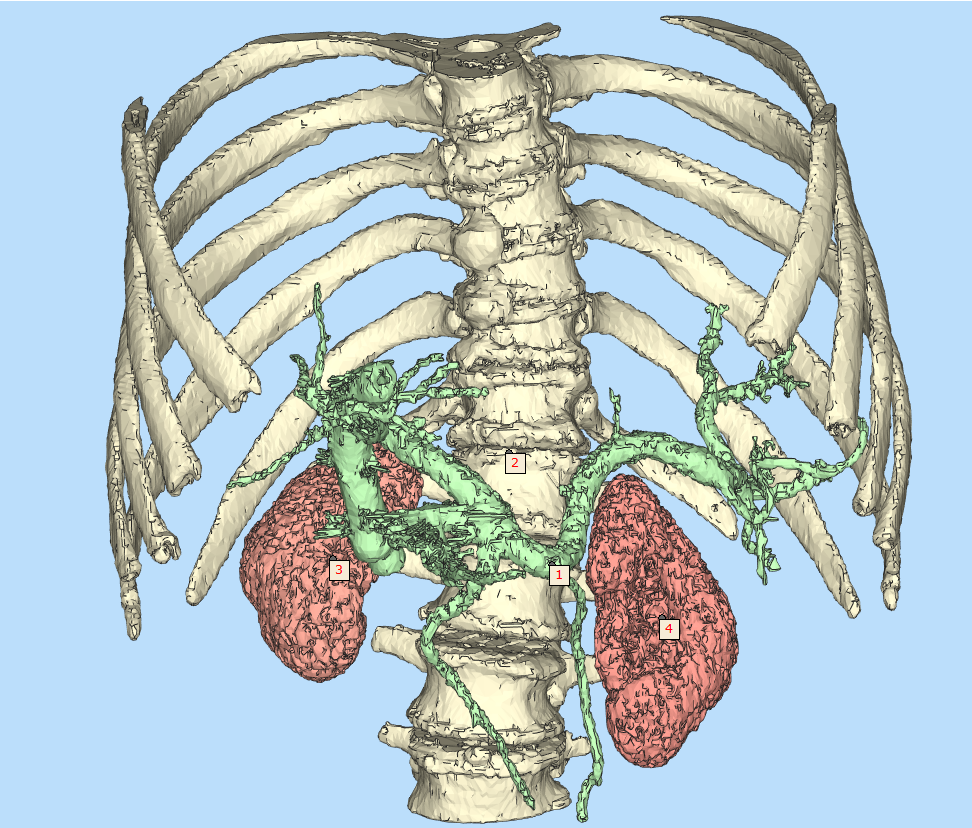
Medical image segmentation involves the extraction of regions of interest (ROIs) from image data, for example from Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) scans. The main goal of segmenting this data is to identify areas of the anatomy required for a particular study or further analysis, such as, to simulate physical properties or virtually positioning CAD-designed implants within a patient. As a result, manual medical image segmentation is a time-consuming task. However, recent advances in AI software are making it easier for routine tasks like this to be completed quickly without compromising on quality.
Benefits of medical image analysis in practice
Medical image analysis is undoubtedly one of the most important procedures performed by radiologists and medical physicists. Accurate depiction of abnormal tissue is key in defining the treatment pathway or drug discovery trajectory, as it enables professionals to quantify and monitor the treatment’s efficiency and patient’s response.
As a direct example, let’s assume that we want to understand the volumetric characteristics of a brain tumour in a longitudinal study. In this study, a patient was repeatedly scanned, and several MRI scans were manually reviewed by a human reader. In the perfect world, an observed decrease of the tumour volume captured would mean that things are going well, but this decrease can easily be a result of poor reproducibility and intra-rater variability, inherently related to manual image analysis.
This is where AI comes into play. As a robust software tool that can automatically deliver, in a fully reproducible way, AI can analyse and provide objective, repeatable measurements of the regions of interest instantly with little to no room for error.
The future of medical image segmentation
AI algorithms help us to not only build automated pipelines for the most time-consuming tasks, such as medical image segmentation, but they can also help healthcare professionals see beyond the visible through extracting features that are impossible to be seen by humans on their own. However, these tools must be thoroughly verified and validated on large, unbiased sets of data to make them appropriate in clinics, as their results can have significant repercussions. Therefore, having an adequate deep model is a great initial step with follow up actions to include designing and implementing theoretical and experimental validation of the pivotal elements of the processing pipeline in a fully reproducible, quantifiable, and thorough way that is evidence-based.